Scientists in Oregon and Washington may have solved one mystery at the root of some of the more puzzling symptoms of COVID-19. They’ve shown that small pieces of coronavirus can cross into the brain in a similar way that HIV does in its victims.
This discovery could help explain why some people sick with COVID-19 experience long-lasting brain fog and fatigue, among other symptoms related to the central nervous system.
When magnified, coronavirus (SARS-CoV-2) looks like a ball with little spiky nodes all over the surface. Those spikes are made of proteins often referred to as the “S1 protein,” after one of the important components of the spike responsible for grabbing ahold of human cells. This the first step the coronavirus takes to harness healthy cells to make copies of itself and spread throughout the body.
The researchers from the University of Washington School of Medicine and Oregon Health & Science University used lab mice to test if those S1 proteins could actually cross from the bloodstream into the brain itself.
“Everything about the brain is special, including the blood vessels. They’re specially modified so they usually keep things out of the brain,” said UW Medicine’s Bill Banks, who works at the Seattle Veterans Affairs Medical Center. “Every once in a while, there’s something like a virus or bacteria or parasite that figures out how to trick its way (through) the blood-brain barrier to get in.”
From their previous research the scientists knew a protein associated with the HIV virus could do this, and now they’re the first to show coronavirus S1 protein can do the same.
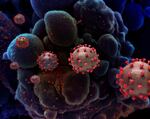
The red spikes on coronaviruses are where S1 proteins are found.
National Institute of Allergy and Infectious Diseases, NIH
“The viral protein can get in. That means that probably the viral protein is causing problems once it does get in. And it also means that probably the virus could get in a well,” he said.
The researchers also found that the S1 protein enters the brain about 10 times quicker through the blood as it does through the olfactory nerve in the nose.
This new understanding of how coronavirus works provides insight into why some people experience brain-related symptoms after becoming infected.
“This study suggests that S1 in mice definitely can enter the brain and could cause immune-related problems, inflammation,” said Jacob Raber, a neuroscientist at OHSU. “It’s important to know because when you know how it works, you can start trying to treat it.”
Neurologist Jennifer Frontera with NYU School of Medicine, who was not involved in the research, says there’s a lot of interest right now in figuring out how COVID-19 affects the brain. Focusing on how the S1 protein works only beings to answer those questions.
“I think most people are interested in what the actual virus might do if it were to cross the blood-brain barrier,” she said.
Frontera says it’s still too early to attribute long term neurological symptoms of COVID-19 to the presence of coronavirus or its S1 protein in the brain.
But if the inference of the paper authors are correct, and the spike protein can cause inflammation in the brain, then some of what doctors are seeing in their patients starts to make sense.
“When there is inflammation in the brain, we think about short and long term effects,” OHSU’s Raber said. “We’re concerned that the S1 protein in the brain might cause long term consequences and therefore have chronic effects as well.”
The research was also able to show a possible genetic explanation for why men and women experience different susceptibility to coronavirus. Raber says their next step is to look at whether men, who as a group experience more severe symptoms of COVID-19, are more likely to experience the neurological effects of the disease.
The research was published this month in the journal Nature Neuroscience.

