Oregon Gov. Kate Brown announced a new strategy Monday to create more desperately needed hospital capacity for a growing number of coronavirus patients, including joint operations by the Portland metro area’s hospitals, the delay of elective medical treatments and the pursuit of additional patient capacity in non-hospital settings.
The effort will bring together Oregon Health & Science University, Providence, Kaiser Permanente and Legacy Health under a joint command to maximize their capacity to treat the surge of patients expected in the weeks to come.
“Metro hospitals will act as one, large unified hospital system for the treatment of COVID-19," Brown said at an afternoon media briefing. "we will expand bed capacity by adding beds in non-hospital settings."
Related: Oregon Orders All Restaurants And Bars To Restrict Access, And Bans Groups Larger Than 25
Oregon hospitals are reducing elective surgeries and discharging patients who can safely recover at home in an effort to free up beds for a potential surge of coronavirus-infected patients.
Dr. Renee Edwards, the chief medical officer at Oregon Health & Science University, told reporters that delaying elective medical procedures would be an important part of increasing hospital capacity for COVID-19 patients.
"All of our institutions are looking at what surgical procedures or what clinical interventions make most sense to tell our patients, 'this can wait,'" she said.
Oregon has 6,601 staffed hospital beds. Edwards said Oregon may need an additional 1,000 staffed hospital beds, including 400 more intensive care unit beds, to accommodate the expected surge of COVID-19 patients.
Hospitals throughout the country are facing shortages of beds and life-saving equipment. According to data from the Kaiser Family Foundation, the average number of beds per person was 2.4 per 1,000 in 2018. And the number of hospital beds has been declining steadily, from about 3 per thousand in 2000.
Oregon, in particular, faces an uphill battle. Oregon has the smallest number of hospital beds per-person in the country: just 1.6 beds for every 1,000 residents.
Oregon and Washington rank last among all states in hospital beds per person
With fewer than two beds for every 1,000 residents, Oregon and Washington each have less than half the capacity of leading states.
Source: Kaiser Family Foundation
Brown's other announced coronavirus measures on Monday were indirectly aimed at easing the crush of patients seeking hospital care as the pandemic hits Oregon. By banning gatherings of more than 25 people and ordering restaurants and bars to close or shift to takeout-only food, the governor and her advisers are stepping up the ongoing effort to "flatten the curve." The idea is to slow the transmission of coronavirus to a point where hospitals can manage the influx of patients.
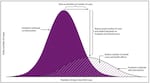
The solid-colored purple curve represents the number of cases over time without intervention. The diagonal-striped curve represents the number of cases over time if protective measures are taken.
The U.S. Centers for Disease Control and Prevention
Brown, Edwards and other state officials who spoke at Monday's news conference said they are pursuing additional beds in a non-hospital setting for expanded patient capacity. But no specifics were addressed.
Former Gov. John Kitzhaber, an emergency-room doctor and nationally recognized healthcare expert, shared a memo Sunday with OPB in which he said the state should be tapping facilities such Portland's unused Wapato Jail, which is currently under private ownership with plans to turn it into a homeless shelter.
Doctors in Oregon and elsewhere have been sounding the alarm about the potential looming bed shortage. They look at what’s happened to healthcare systems in other countries, and it concerns them. In places like Italy, doctors have had to make hard decisions, like determining that patients over 80, who are more likely to pass away from COVID-19, will not receive health care.
But Italy has an average of 3.2 beds for every 1,000 people. If Oregon sees a spike in cases, which models currently suggest it will, the situation could be much worse.
In a letter to the state of Oregon, signed by over 430 Oregon doctors, they wrote. "We see ourselves making decisions in the next two weeks on who will live and who will die because we don't have resources sufficient to care for them."
That is particularly clear in smaller communities. Curry Health Network runs Curry General Hospital in Gold Beach and Curry Medical Center in Brookings, along with several other smaller clinics throughout the area. Jessica Carlson is the president of medical staff for Curry Health Network and the surgeon at Curry General Hospital. She said their network and others like it aren’t set up to handle a deluge of patients like they might see from COVID-19.
Related: A Glossary Of Coronavirus Terms, From ARDS To Zoonotic
“For instance, we usually have a 96-hour restriction on admissions, so we have to try to discharge all of our patients within 96 hours,” Carlson said. That usually involves sending patients who need long-term care to hospitals with more resources.
The governor removed such restrictions on hospitals like Carlson’s but it doesn’t change the fact that they aren’t set up for long-term care.
“We functionally have 16 beds. Five of those beds are in the ER,” Carlson said, “We have two rooms we can convert but we don’t have a standard ICU.”
That means there are already times when there are gurneys and beds lining the hallways.
“Our county has 22,000 people. But, wow, only 16 beds,” Carlson said.
They’re also short on ventilators, which are a critical part of treating patients with coronavirus. At Curry General, they’re mainly used to keep patients alive until they can go elsewhere.
Carlson’s hospital essentially has only one person doing each job, she said.
There are just three physicians at any time for ER and admitted patients," she said. "Just myself, one ER physician, and a hospitalist. That’s it.”
PeaceHealth Sacred Heart Medical Center at RiverBend in Eugene is the primary hospital for the southern Willamette Valley area and surrounding areas, with a few smaller satellite campuses. It has 347 licensed beds. It also has the highest occupancy rate in the state - 96.6% in 2018.
To prepare for a potential surge of cases, RiverBend has been setting up tents and trailers outside of the hospital to help triage potential patients.
In a statement the hospital wrote: “please note that this is part of our preplanning efforts and we do not currently have capacity issues. We are preparing for a potential future state as the need may arise.”
That’s what all hospitals are doing right now: prepping for future capacity issues. But the question remains: if Oregon has the worst bed-to-person ratio in the country, why? It may just be a matter of unexpected population growth, as was the case the area served by RiverBend. But when asked the question in a press conference, Oregon Health Authority Director Patrick Allen said that the low number of beds in Oregon isn’t reflective of a bad healthcare system, it’s reflective of a good one.
Allen said Oregon is able to keep the overall bed number so low “by providing access to primary care so that people don’t require hospitalization, so we’re able to save costs and the healthcare system.”
When asked if that puts Oregon in a worse position in crises like this, Allen said, “Well, it’s hard to argue that we should keep people sicker so that we can have the hospital beds, right?”
But the idea that early intervention and primary care is keeping people out of hospital beds is not reflected in the experiences of doctors and nurses, who say the trend for the last ten years has been one of trying to do more with less.
Hospital beds per person are on the decline.
As the population Oregon and Washington increases, the number of hospital beds has not kept pace. The US as whole also has a declining number of beds per person.
Source: Kaiser Family Foundation
It’s not reflected in the data, either. The number of total staffed beds in Oregon has grown very slowly, but steadily since 2012. But the percentage of those beds that are occupied has grown even faster, according to OAHHS data.
In Monday's news conference, Brown said she’s asked the federal government for help. On March 3 she put out a request for an additional $7 million to $10 million per month in aid from the federal government. About 10% of that has arrived so far and she expects more later.
But in a call Monday, President Trump told governors that if they want additional help they should try to find it on their own, first. Especially when it comes to lifesaving equipment like respirators and ventilators, which Brown also requested from the federal government. Oregon only has 688 ventilators in the entire state. They help people with compromised lungs breathe and can be the difference between life-and-death for patients.
In the search for more doctors, more nurses, more ventilators and more beds, Oregon will face steep competition. Because while Oregon might have the worst person-to-bed ratios in the country, the United States has one of the worst ones in the entire world.
Oregon and Washington are last in the US. The US is behind 30 others.
Leading countries have more than 10 beds for every thousand residents. The U.S. has fewer than three.