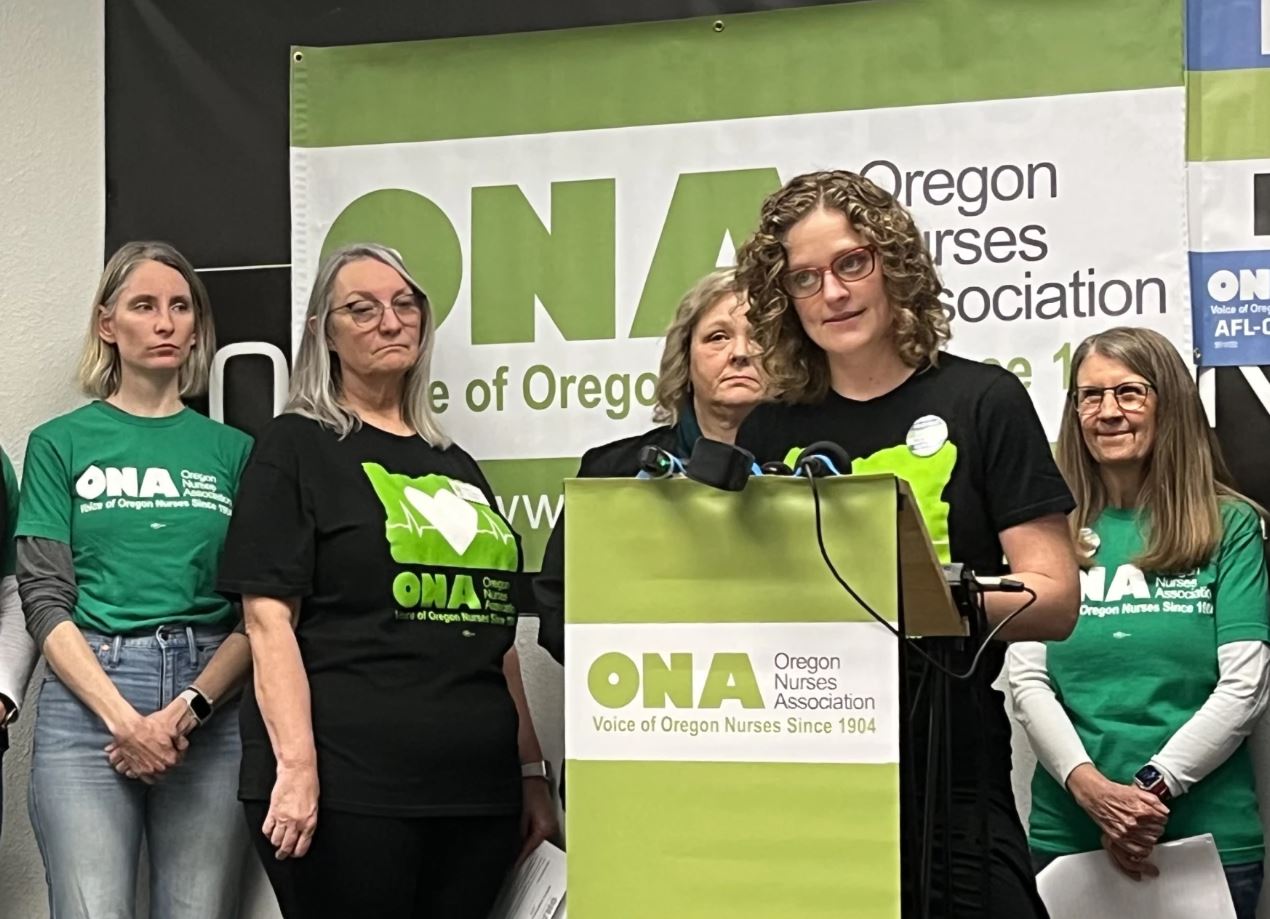
FILE - Heather Herbert, a hospice nurse with PeaceHealth, speaks at a press conference in Springfield, Ore., on Dec. 29, 2023.
Nathan Wilk / KLCC
After almost a year of negotiations, nurses with PeaceHealth Sacred Heart Home Care Services are going on strike. More than 90 nurses with the Oregon Nurses Association will be striking for two weeks starting Feb. 10. These nurses provide hospice care and other services to patients in the Eugene area.
The nurses have been working under an expired contract since April 2023 and are looking to raise safety standards, increase recruitment and retention, and secure better pay.
Heather Herbert is a hospice nurse with PeaceHealth and an ONA member. She joins us to share more about her job and nurses’ hopes for the future.
In a statement to OPB, PeaceHealth officials wrote:
“After notifying the ONA that their initial strike date of Feb. 1 would cause a lapse in benefits for their members, the union pulled their initial notice and filed for the new strike date of Feb. 10. PeaceHealth notified the union of their error to prevent caregivers from unnecessarily losing their health benefits due to the strike timing. PeaceHealth’s employment policy states that benefits expire the last day of the month in which you work – i.e. if an employee’s last day of work is Jan. 31, their benefits expire at the end of January. If an employee’s last day of work is Feb. 1, their benefits expire at the end of February.
“Once PeaceHealth received the strike notice from ONA, we immediately postponed our upcoming bargaining sessions to focus our full attention on ensuring the continued delivery of safe, high-quality patient care during the union’s strike. We look forward to resuming negotiations at a later date, but right now our focus must be on our patients and providing uninterrupted care.
“As is standard practice, PeaceHealth has contracted with an agency to provide experienced temporary replacement caregivers during the strike to ensure patient care continues uninterrupted. This strike will not impact operations at PeaceHealth hospitals and clinics in Lane County. PeaceHealth has successfully negotiated four other long-term union contracts over the last 12 months – including one with ONA – providing wage increases and stability for nearly 3,000 caregivers in Lane County.”
The following transcript was created by a computer and edited by a volunteer:
Dave Miller: This is Think Out Loud on OPB. I’m Dave Miller. After almost a year of negotiations, nurses with PeaceHealth Sacred Heart Home Care Services are going on strike on Saturday. These nurses, about 90 of them, provide hospice care and other services to patients in the Eugene Springfield-area. They’ve been working under an expired contract since April. The planned strike is scheduled to last for two weeks. Heather Herbert is a hospice nurse with PeaceHealth and a member of the union, the Oregon Nurses Association. She joins us now. Heather, welcome.
Heather Herbert: Thank you. It’s great to be here, Dave.
Miller: Yeah. Thanks for joining us. For our listeners who may not know what your work is like, can you just describe, first of all, just the range of patients that you might see?
Herbert: Yeah. We work closely with Home Health, so they’re also in this bargaining that we’re doing, but I’ll speak mostly about hospice. To come onto our service, you have to have two doctors agree that if you were to die in six months, no one would be surprised and we don’t do anything to hasten death, nor do we do anything to prevent it. We just kind of let nature be there and then we just work with families and patients to support them with symptom management and whatever else they need to have the best quality of life at the end of their life.
Miller: What kind of care might they require? What kind of care might that entail?
Herbert: So a lot of it is things like pain, shortness of breath. As our bodies start to fail, all of our systems start to. It could be anything with your disease process. So seizures or edema. We’ll put in drains to help drain people’s fluids in their lungs or abdomen or their kidneys. You name it. Those are the types of things that we do.
Miller: I mean, the timing is pretty squishy, right? Just based on what you said, that people wouldn’t be surprised if somebody died within six months. But I imagine that means that you might have a patient for three days, but you could also have them for more than a year?
Herbert: Yeah, we’ve had patients for many years, and we grow very close with them, because we’re in their home multiple times a week, usually, during that time. And we also work with moms who know that their babies won’t live for very long as well. So it’s the whole range of anybody who would qualify, can be a part of our service.
Miller: Maybe this is just my own assumptions that are incorrect, but that strikes me as maybe the most challenging part of your job, dealing with a newborn who is going to die soon, as opposed to somebody who’s 90. Is that accurate?
Herbert: Yeah. That’s accurate. I work a lot with kids and so we get to partner with parents who are saying hello to their new person and also goodbye at the same time. And what fears do they have? What are they wanting to experience at this time? And help partnering with them to reach their goals.
Miller: One of the issues, to turn more towards the bargaining, is the work that you do and the work that happens by nurses, in the hospital context. What’s the overlap, in terms of the care that you and your home-based colleagues are providing and what’s being provided by nurses, in a hospital setting?
Herbert: Yeah, I love this question. I have worked in the hospital. I was on the oncology floor. I’ve worked in the OR, I have used every single one of my same skills, from IVs, wound care, catheters, medications. And as a hospice nurse, I still use all of those same skills. I have to have the same degree, the same level of education. But in the hospital, things are very much controlled. You have your hospital room, you get to come in and out of that room at any time of the day. We tell people what to wear. Here’s your gown, go sit over there, here’s your OMRON number that we’ll monitor you through.
With home care, we are a guest in someone’s home and I come into that home, whether it is a mansion on a beautiful hill or a broken down RV, or a tent. I’ve been in homes with no running water, no floors, people who don’t speak English and I don’t necessarily have an interpreter that I can call easily to come and meet me there. And all I have are the tools in the back of my car and to help provide the exact same care that I have given in the hospital.
Miller: What drew you to this particular version of nursing? I mean, because as you said, you’ve worked in hospitals before. I assume you sought this out?
Herbert: Yeah. Well, my last job was in the OR and I just really missed patient care. And what I love about my job is I get to go into people’s homes and I get to see the essence of who someone is. It is a very intimate setting and people are usually scared, and I get to meet their family and their goals. I partner with them to make their last chapter of their life the best chapter that we can give them.
Miller: Let’s turn more fully then to the negotiations. They’ve been going on for just about a year now. What are the biggest sticking points right now?
Herbert: Well, it’s actually been over two [years]. We’re going on our second year now and all that we are wanting is to have the same pay, the same that we’ve always had. We’ve always had the same exact contract with the hospital as before. And so all we’re asking for is equal treatment that they’ve done before, since we’re doing equal work. And this has just been the standard.
Miller: So, meaning in the past, you have been paid the same as hospital-based nurses. And you’re saying that that’s what you want right now.
Herbert: Yeah, that’s what we want right now. And the reason that it’s so important is because our nurses are leaving, and if you don’t have the staff, then your organization is no longer functional. And I have always loved that the culture of where I work, I can go into the spaces of people’s homes and just be present and be what they need, while providing the same care that they get in the hospital. But now, we have a bunch of nurses who are leaving and we can’t bring in new ones. I’m no longer able to provide the same type of care that I love so much.
Miller: You mean, because you’ve had to take on more patients? Because some nurses are leaving, the care that you’re providing has to change?
Herbert: Well, currently, two nurses that normally work alongside me are not working. So I have to take on their role as well. In the past, I’ve been able to call my scheduler and say, this family is in crisis and I need to stay here, and they used to be able to give those visits to other nurses. And now they’re not able to do that because they don’t have the staff. People are leaving because they can get paid more elsewhere.
Miller: How much turnover has there been among home-based hospice nurses over the last year or two?
Herbert: We’ve never had a retention problem before. We’ve always been able to keep our nurses and hire quickly. And within the last year, there’s been about 30 nurses who have left, which when you’re talking 90 nurses, that’s substantial and it takes months and months to train new nurses. We’re just not able to hire. Nobody is applying.
Miller: Where have they gone? What’s the range of places they’ve gone to?
Herbert: Some of them have gone into the hospital, into mental health. They’ve gone into insurance companies, I believe. Those are some of the few.
Miller: Do you see that exodus as being tied specifically to the ongoing labor negotiations? Or just a separate fact that’s complicating your life right now, based on other issues about the challenges of the job or the desire to have the stability, maybe, that would come from other kinds of jobs?
Herbert: Working with my fellow nurses, we love our jobs. We love the beautiful, sacredness of caring for dying people and the relationships that we get to build with the family. And we’ve never had a retention problem before. Since this negotiation has started, it feels like divorce has happened in our unit. It feels like we’re divided. We’re not being treated with respect, things are being dragged on for a really long period of time. People are crying in the office because of the strike that we’ve decided to do because our loyalty is to our patients. And if you can’t provide the care that you’re wanting to, it causes a lot of moral distress.
Miller: Have you thought about leaving the profession or at least leaving this particular position?
Herbert: I have. I totally have. I’ve applied at different places and I’ve chosen to stay because when you care for people this way, I don’t know how to go back. I don’t know how to hold the hand of a dying person and look them in the eyes and feel so connected and bring peace to a family who is so scared of the most important moment of someone’s life. It’s very rewarding and I don’t know how to go backwards.
Miller: Go back to a knee surgery…
Herbert: I don’t know how to go back to the OR, where it feels like an assembly line of just people coming in, people going out.
Miller: I mean, I’ll just say that obviously for those people who are going in for those surgeries, it’s very important for them in that moment as well. But I think our listeners take your point.
We did reach out to PeaceHealth officials and they gave us a statement. It reads in part, “Once PeaceHealth received the strike notice from ONA, we immediately postponed our upcoming bargaining sessions to focus our full attention on ensuring the continued delivery of safe high quality patient care, during the union’s strike. We look forward to resuming negotiations at a later date. But right now, our focus must be on our patients and providing uninterrupted care as is standard practice.”
They wrote, “PeaceHealth has contracted with an agency to provide experienced temporary replacement caregivers during the strike to ensure patient care continues uninterrupted. The strike will not impact operations at PeaceHealth hospitals and clinics in Lane County.”
Heather Herbert, have you talked to your patients about the strike?
Herbert: I have spoken to them and it’s a really hard conversation because our loyalty is to our patients. And we have personally dedicated our hearts and our times into partnering with them and walking this journey with them. And it feels so sad that we can’t be there during this time.
Miller: What have you heard in response from them?
Herbert: From our patients?
Miller: Yeah.
Herbert: A lot of them can’t get out of bed. And most of them wish that they could stand with us because they know that we are doing this for them and our community so that we can build a stronger hospice service, to be able to give back to them.
Miller: What normally happens when one nurse leaves for the day and then another nurse takes over? What kind of a handoff is there normally?
Herbert: So we have patient charting that’s available for people to read with notes of like, to-do lists, things like that. And then we also get together every other week with all of the team and talk about all of our patients with the social workers and chaplains so that we’re together. Life happens unexpectedly, but things that may happen down the road, say, somebody needs respite or we’re worried about a pain crisis or they’re going to be homeless, or stuff like that. How do we, together, support the upcoming needs that people may have?
Miller: Is there going to be anything like that, any kind of warm handoff, between you and your fellow nurses, and what PeaceHealth calls temporary replacement caregivers?
Herbert: I wish that there were. Yesterday was my personal last day, and they haven’t told us who the nurses are who are coming. So I wouldn’t know who to give the report to.
Miller: Why did the union put an expiration date on the strike? It’s planned to start in two days, on Saturday, and to last for two weeks.
Herbert: We’re nurses and we’re just like everyone else out in the community. We have our own responsibilities to our families. A lot of us are single moms. We need our insurance. That was a big concern that a lot of people have. Some of their children are medically fragile and they need to be able to go to a doctor’s office, or older spouses who need that. So we are just hoping that this strike lets PeaceHealth know that we are very serious about how we feel about what the culture is of our community, the hospice, so that we can give the best to our community, but still be able to keep our insurance and things like that. And get back to our patients, because we care about them.
Miller: Just to go back to your own work and your own way of thinking about life now, I’m curious if being a hospice nurse has affected the way you think about your own death?
Herbert: Absolutely. I’ve actually done the practice. People have birthing plans and not everyone always talks about a death plan. So I’ve actually done my own death plan about where I would like to be, what music I’d like, things like that. But also I think it’s just made me a better person in general, being able to see what families go through. It reminds me that life is really precious. So I take more opportunities to love the people that I love and forgive easier and to laugh faster, quicker, and to not take life for granted.
So this job has definitely changed me, makes me a better listener. That’s what I say when I’m like, “I don’t know how to go back,” because I’m a better person for being this type of nurse.
Miller: Heather Herbert, thanks for your time today. I appreciate it.
Herbert: If anyone would like to come and join us, you’re more than welcome to come and join us on the 10th, and then respectournurses.com is where we have some really good information.
Miller: Heather Herbert is a hospice nurse with PeaceHealth Sacred Heart Home Care and a member of the Oregon Nurses Association.
Contact “Think Out Loud®”
If you’d like to comment on any of the topics in this show or suggest a topic of your own, please get in touch with us on Facebook, send an email to thinkoutloud@opb.org, or you can leave a voicemail for us at 503-293-1983. The call-in phone number during the noon hour is 888-665-5865.


