This story has been updated.
More than 1,800 Providence health system nurses and home health workers ended their weeklong strike at 5 p.m. Friday. It was the first major health care worker work stoppage in Portland in more than 20 years.
But it may not be the last.

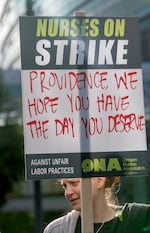
Nurses picket in front of Providence Portland Medical Center, Monday, June 19, 2023.
Kristyna Wentz-Graff / OPB
Experts say nurses unions across the country have been more willing to authorize strikes and to stop work in the last year due to lasting exhaustion from the pandemic and an unwillingness to continue putting up with existing working conditions.
That’s pushed more nurses to accept the risks inherent in a strike: loss of pay, the stress of walking away from patients, and the question of how the public will perceive a strike by health care workers, who are comparatively well compensated.
Heronia “Ro” Woodward is a home hospice nurse who works in East Portland. On Monday morning, along with dozens of colleagues, Woodward picketed outside the small office park in Northeast Portland that is the main office of Providence’s home health and hospice team.
The atmosphere was festive. Passing drivers honked and cheered the nurses. There were donuts, and a Tracy Chapman song playing.
Woodward was thinking of her patients, who she’d last seen the Friday before the strike.
“So much can happen in just 24 hours,” she said. “A patient can be stable today, and then tomorrow, they are in a pain crisis.”
Providence hired temporary nurses from across the country to keep the hospice team staffed during the strike. So Woodward knew her patients were being cared for. But, she said, the replacement workers don’t know those patients like she does, and she believed they are not getting the same quality of care.
“That’s heartbreaking to me,” she said.
Still, Woodward said the strike was necessary. She said she was standing up both for herself and her patients “so that in the future they get the care that they need, and we get the … I will say the financial recognition and the benefits that we deserve as well.”
A debate over pay, and more
At the simplest level, this week’s strike was a dispute about compensation for health care workers. The nurses and home health workers are asking for a wage hike, more time off, and double pay if they come in last minute to cover a shift that is short-staffed.

The picket line at Providence Portland Medical Center, Monday, June 19, 2023.
Kristyna Wentz-Graff / OPB
It’s unclear to what extent this strike was part of a calculated strategy on the part of either side, and if so, who should be considered responsible for it.
What is clear is that the Oregon Nurses Association delivered a 10-day strike notice earlier this month after a difficult bargaining session with Providence that had dragged on until 3 a.m. The union hoped the escalation would give them more leverage, and wanted to keep negotiating. That didn’t happen. Providence canceled the remaining bargaining sessions and began preparing to bring in a temporary workforce.
For about a decade before the pandemic, nurse wages and benefits were relatively flat, according to Christopher Friese, a professor of nursing and health management and policy at the University of Michigan. Health care systems were trying to run lean, he said. And unions were more likely to try to reach a quiet deal rather than strike.
He said that’s changed after nurses’ experience on the front lines of COVID-19, in some cases risking their lives and their families’ health to do their jobs.
“Nurses were asked to do the unimaginable — for years,” Friese said. “And so now they’ve had time to think about what they’ve been through and where they were even before the pandemic — and more and more nurses are saying enough is enough.”
There have been strikes in Washington, California, Minnesota and New York over the past year. And, Friese said, nurses are using these strikes to talk about more than just their wages and benefits, they’re also raising questions about the safety and quality of the care they provide.
That’s been a talking point on the picket line in Portland. Representatives from the Oregon Nurses Association, which represents Providence’s health care workers, say hospitals have under-invested in nursing and that affects patient care. They argue nurses are now handling a post-pandemic population that is sicker, misusing substances more often and harder to treat.
What’s best for patients?
This week’s strike included nurses at Providence’s small hospital and clinics in Seaside and nurses at Providence Portland Medical Center, the health system’s second-largest hospital in Oregon. It also included the 400 or so nurses, social workers, and physical therapists with the Providence Home Health and Hospice team. They say the central disagreement in their contract negotiations is over their increasing workload and the problems that it creates for patient safety.
“They have not hired enough nurses,” said home health nurse Peter Gerber. “I’m doing the work of two and a half nurses.”
Gerber has been a home health nurse for Providence for eight years. He cares for people who live in his own Beaverton neighborhood.
“I take care of those people around the corner, down the street who can’t leave their homes,” he said, “who are stuck in bed, who have dementia, who can’t talk.”
Aishia Sorbets, a registered nurse in the cardiac telemetry unit, pickets at Providence Portland Medical Center, June 19, 2023.
Kristyna Wentz-Graff / OPB
Gerber said his normal caseload used to be about 25 patients, which he says is best practice. But over the past year, his caseload has surged as colleagues have left or retired. Two months ago, he hit 44 patients.
“I’m not able to see those patients as frequently as I should to notice the changes in their wounds, in their breathing, to help people stay out of the hospital,” he said.
He’s also expected to meet daily productivity targets. Generally, that means visiting five to six patients a day. An easy patient might take just an hour. But a complicated patient can take up half a day. He can miss his target if anything unexpected slows him down, like a traffic jam, or having to go out of his way to find a place to pee.
“I just want to go to the bathroom,” he laughed, explaining that he knew where to find all the Goodwills in his coverage area because he’s found the stores to have the cleanest public restrooms.
If health care workers are feeling newly emboldened to strike, health care systems have an obvious reason to dig in and avoid making concessions during bargaining. Many are losing money and under pressure to try to contain costs.
According to financial statements, Providence Health and Services lost $345 million on its operations in the first quarter of this calendar year, an improvement over its performance last year.
“Hospitals across the country are under siege financially,” Friese said. They’re looking for every opportunity they can to support their budget and that’s appropriate. If hospitals continue to run a deficit, the hospital doesn’t exist.”
Nursing is an obvious expense to consider for executives trying to balance a budget because it can make up around a quarter of a hospital’s expenses.
If you take a broader look, Friese argues, investments in nursing pay off in the long run.
“You have fewer complications, you get patients out of the hospital sooner, you avoid deaths and you actually keep your nursing workforce,” Freise said.
Back to work, with no deal yet
Providence officials declined an interview request for this story. In public briefings during the strike, they’ve repeatedly declined to say how much the strike is costing in replacement workers and postponed surgeries. Providence says it’s been able to manage for 5 days without compromising patient safety.
Providence Portland Medical Center has been operating at 75% capacity for the week, while the much smaller Seaside hospital was running at half capacity. All non-critical surgeries had to be rescheduled. But by the end of the week, the Portland hospital was running smoothly enough to reopen its NICU and start accepting patient transfers again
Spokespeople have responded to some questions in writing. They say that the nurses who are striking earn more than $100,000 a year on average, and get at least five weeks of paid time off to start — that count includes vacation, sick leave and holidays. The union has disputed some of these numbers.
At a press conference, Jennifer Gentry, chief nursing officer for Providence’s central division, pointed out that Providence supported legislation the nurses union wrote that will mandate minimum staffing levels in Oregon hospitals starting next year - though not for home health workers. Lawmakers approved that bill Thursday, and it’s headed to Gov. Tina Kotek for her signature.
“We do believe in safe staffing and high-quality patient care, for all of our patients regardless of the setting,” Gentry said.
And Gentry agreed that in the aftermath of the pandemic, Providence, the fourth largest health system in the country, has struggled with working conditions for its nurses. Gentry said the system is starting to improve, though, with higher retention and lower turnover. She hopes both sides can come back to the table in good faith next week.
“I think the strike has been very disruptive and emotional and expensive for all parties involved,” Gentry said.
The strike officially ended Friday evening. Temporary workers stayed on until their contract ended at 7 a.m. Saturday, and then staff nurses returned to work.
On Friday, however, the Oregon Nurses Association held a press conference accusing Providence of violating state employment law during the strike, claiming the company’s hiring of nearly five hundred temporary replacement nurses violated a law prohibiting employers from using professional strikebreakers.
At a press briefing Saturday, Providence acknowledged it acquired temporary staff through U.S. Nursing, a company that specializes in providing temporary staff during labor disputes.
Providence said the alternative would have resulted in hospital closures. During the briefing, Gentry and other Providence representatives emphasized that life-saving procedures continued at the nonprofit health company’s facilities during the strike.
“It would be incredibly challenging, if not impossible, for us to have sourced 500 nurses to come here within 10 days notice for this strike,” Gentry said. “It’s important to us that we continue to focus on patient care and keep our doors open.”
Providence and the nurses association are scheduled to resume contract negotiations for home healthcare and hospice nurses on Tuesday. They have not yet scheduled dates to resume negotiations for hospital workers.
