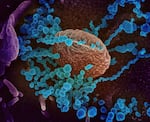
This scanning electron microscope image shows SARS-CoV-2 (round blue objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19.
NIAID-RML
Brian O’Roak is in a race against the COVID-19 virus — or, to be more specific, a race against the virus’s evolution.
Like all viruses, the COVID-19 virus mutates as it replicates, accumulating about one change in its viral genetic code every two weeks. Many of those mutations are evolutionary dead ends that take the virus nowhere. A few help it survive by making it better at infecting us.
And O’Roak, co-director of the SARS COV-2 Genome Sequencing Center at Oregon Health & Science University, is trying to find those variants in Oregon to help slow their spread.
This fall, two things happened that profoundly changed the nature of his work and the pandemic itself.
Cases of COVID-19 surged worldwide and in Oregon, giving the virus billions of opportunities to replicate itself and mutate. And variants of concern emerged in the United Kingdom, South Africa and Brazil that seem to have an edge over the parent version of COVID-19.
The U.K. variant is more easily transmitted between people, and more deadly, but the current vaccines work well against it. Scientists are increasingly concerned, though, that the variants that originated in South Africa and Brazil are better able to infect people who have been vaccinated and to re-infect people who have recovered from COVID-19.
O’Roak now spends much of this time helping Oregon search for these new variants. Last month, as he was helping investigate an outbreak of COVID-19 in Marion County, he found a viral genome that surprised him: the U.K. variant of COVID-19, with an additional mutation known as E484K.
It’s a hallmark mutation of the virus’s spike protein that some scientists have nicknamed “eek.”
“That was particularly surprising and worrying to us because that is a mutation that is very prominent in the other variants of concern,” O’Roak said.
E484K is found in both the South African lineage and the Brazilian lineage of COVID-19, and scientists believe it is one of the mutations that helps those variants evade antibodies.
“It’s the marker of a potentially scary virus,” said Bill Messer, an assistant professor and colleague of O’Roak at OHSU whose career has focused on virus evolution.
The scientists don’t yet know what their discovery means because they’ve only found a single example of it in Oregon.
But it’s part of a much larger global story of viral evolution — and our response — that lies at the heart of the most important question about the pandemic: Will we eradicate COVID-19 for good, or will it be something, like the flu, we live with and die from every year?
Where did the new variant come from?
In mid-February, O’Roak’s team began working on some samples they’d received from a large outbreak of COVID-19, involving more than 20 cases, in a health care setting in Marion County.
The Oregon State Public Health Lab referred the samples to O’Roak’s team after OHSU agreed to help the state sequence high-priority samples.
They received eight samples from the outbreak and were able to sequence viral genomes from seven of them. As they expected, six of the samples were the more contagious B.1.1.7 variant that originated in the United Kingdom.
But one sample was different: it had an extra mutation affecting its spike protein, E484K.
This specific combination of mutations has recently been discovered elsewhere. Since January, scientists in the United Kingdom have identified more than 50 cases of the same novel combination — which has been dubbed a new variant of concern. But the sample sequenced from Marion County was the first time the new variant was reported in the United States.
O’Roak is confident that the variant is homegrown: It arose spontaneously in Oregon, as the B.1.1.7 virus replicated during the outbreak under investigation.
He says a distinct parent version of B.1.1.7 present in the samples from the outbreak is also present in other samples from the community in Marion County, but without the E484k mutation.
“That was one of the pieces of the puzzle that led us to believe that the mutation arose during the outbreak,” he said.
The OHSU scientists aren’t identifying the specific location of the B.1.1.7 outbreak. The Marion County Public Health Department declined to comment on whether the outbreak involved people who’d been fully or partially vaccinated and whether it is ongoing.
The Oregon Health Authority also declined to comment on the outbreak. Health authority officials wouldn’t answer specific questions about if the state is taking additional steps to investigate the mutated virus, to sequence more samples from the outbreak or to ensure the mutated version of B.1.1.7 doesn’t spread.

Andy Fields and Sally Grindstaff prepare to load a SARS-CoV-2 sequencing run at Oregon Health & Science University.
OHSU
“When OHA is notified about a variant of concern, we enter the information in the disease tracking database so that all case investigators working to respond are informed,” Oregon Health Authority spokesman Tim Heider said.
The agency also gave examples of the typical support it provides during COVID-19 outbreaks in congregate care settings, including providing testing, personal protective equipment, and monitoring isolation and quarantine procedures.
The OHSU team said it hopes to do more genetic work on the outbreak in Marion County to see if the mutated B.1.1.7 variant has spread. That could clarify whether what they’ve discovered is a single fascinating example, or a new variant circulating locally that public health departments in Oregon should be prepared to see.
“The problem is, we don’t know,” Messer said. “At this point there’s just the single sequenced virus that carries this extra mutation.”
There’s a lot we don’t know about variants and vaccines
So there’s no evidence, at least not yet, of the variant discovered in Oregon spreading locally.
There’s also no direct evidence that it is less susceptible to the vaccines currently being deployed to stop the pandemic, though indirect evidence suggests that could be the case, according to the OHSU team.
Because the same variant emerged a while ago in the United Kingdom, scientists there have already begun to test how it behaves in laboratory experiments. Messer and O’Roak caution that the data from these early studies hasn’t been peer reviewed yet. Still, what that data shows concerns them.
In those experiments, antibodies were significantly less effective at neutralizing the combination virus — B.1.1.7 plus the E484K mutation — than they were against the the parent strain used to derive our current vaccines, or the B1.1.7 virus without the added mutation.
Also concerning is the reduced performance of vaccines that have been tested in trials in South Africa while the B.1.351 variant, which includes the E484K mutation, was circulating there.
For example, in clinical trials, the Johnson & Johnson vaccine was less effective at preventing infection in the trial’s participants in South Africa than it was for the trial’s participants in the United States. In South Africa, an overwhelming majority of the samples Johnson & Johnson sequenced for its trial identified the B.1.351 variant. The vaccine did provide strong protection against severe illness and death, however, even among the participants in South Africa.
“I think everyone on our team can agree that we don’t want this variant spreading through our community,” O’Roak said.
Next steps: Vaccines, masks, handwashing and distancing
So, how do we stop it?
The answer isn’t complicated: The same simple steps public health officials have been suggesting for a year now prevent transmission of the virus and its variants. That means wearing a mask, maintaining a safe distance from others in public and avoiding large gatherings.
“The spread of these variants is not an inevitability,” Messer said.
Getting vaccinated as quickly as possible is also critical. All three vaccines currently available in Oregon offer very substantial — if imperfect — protection against infection, including from variants.
Masking, distancing, getting vaccinated. All are strategies to protect yourself, your family and your community. But they’re also critical strategies to slow down the path of COVID-19′s evolution.
It’s an argument a group of scientists made this week in a paper published in the prestigious journal Nature.
“If the rampant spread of the virus continues and more critical mutations accumulate, then we may be condemned to chasing after the evolving SARS-CoV-2 continually, as we have long done for influenza virus,” they wrote.
“Such considerations require that we stop virus transmission as quickly as is feasible, by redoubling our mitigation measures and by expediting vaccine rollout.”
Messer likens our current moment to the third act of a Shakespearean play. The pandemic isn’t over just because the vaccines have triumphantly arrived on the scene to defeat the virus. The virus is evolving, too. The emergence of new variants that fuel a resurgence of the virus might be act four.
Act five — the resolution of this pandemic — will depend, he said, on the combination of all of our ceaseless efforts to stop it.

